|
 |
Dr. Shelley Sekula Gibbs is an experienced Mohs surgeon.
Dr. Sekula Gibbs is a board certified dermatologist who has practiced Mohs surgery in the Houston area for over 20 years. As a member of the American Society for Mohs Surgery she adheres to high standards for using this highly successful technique. Mohs surgery provides up to a 96%-98% cure rate for primary basal cell skin cancer. And, by creating the smallest possible defect, Mohs surgery patients have an improved opportunity for an excellent cosmetic result.
What is Mohs Micrographic Surgery?
Mohs micrographic surgery is a specialized, highly effective
technique for the removal of skin cancer. The procedure was
developed in the 1950s by Dr. Frederic Mohs at the University
of Wisconsin, and is now practiced throughout the world. Mohs
surgery differs from other skin cancer treatments in that it
permits the immediate and complete microscopic examination of
the removed cancerous tissue, so that all “roots”
and extensions of the cancer can be eliminated. Due to the methodical
manner in which tissue is removed and examined, Mohs surgery
has been recognized as the skin cancer treatment with the highest
reported cure rates and small defects allowing for optimal cosmetic results.
 Special
Qualifications of the Mohs Surgeon Special
Qualifications of the Mohs Surgeon
Physicians performing Mohs surgery should have specialized
skills in dermatology, dermatologic surgery, dermatopathology,
and Mohs surgery. Basic and advanced training in Mohs surgery
is available through selected residency programs, specialized
fellowships, observational preceptorships, and intensive training
courses. In addition, the Mohs surgeon must have the required
surgical and laboratory facilities, and be supported by a well-trained
Mohs nursing and histotechnological staff. Dr. Sekula Gibbs can provide you with detailed information regarding her
training in the above disciplines, as well as all applicable
professional affiliations. To learn more about the American
Society for Mohs Surgery, visit their web site www.mohssurgery.org.
Advantages of the Mohs Surgical Procedure
Some skin cancers can be deceptively large – far more
extensive under the skin than they appear to be from the surface.
These cancers may have “roots” in the skin, or along
blood vessels, nerves, or cartilage. Skin cancers that have
recurred following previous treatment may send out extensions
deep under the scar tissue that has formed at the site. Mohs
surgery is specifically designed to remove these cancers by
tracking and removing these cancerous “roots”. For
this reason, prior to Mohs surgery it is impossible to predict
precisely how much skin will have to be removed. The final surgical
defect could be only slightly larger than the initial skin cancer,
but occasionally the removal of the deep “roots”
of a skin cancer results in a sizable defect. The patient should
bear in mind, however, that Mohs surgery removes only the cancerous
tissue, while the normal tissue is spared.
Special Indications for Mohs Surgery
It is important to note that Mohs surgery is not appropriate
for the treatment of all skin cancers. Mohs micrographic surgery
typically is reserved for those skin cancers that have recurred
following previous treatment, or for cancers that are agressive or at high
risk for recurrence. Mohs surgery also is indicated for cancers
located in areas such as the face, nose, eyelids, lips, hairline,
hands, feet, and genitals, in which maximal preservation of
healthy tissue is critical for cosmetic or functional purposes.
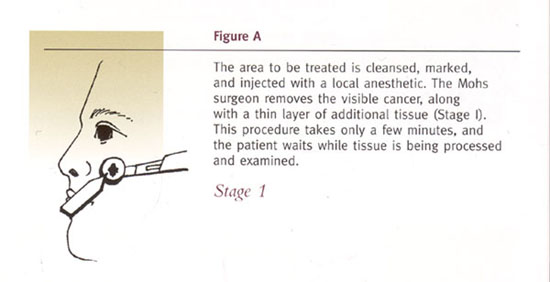
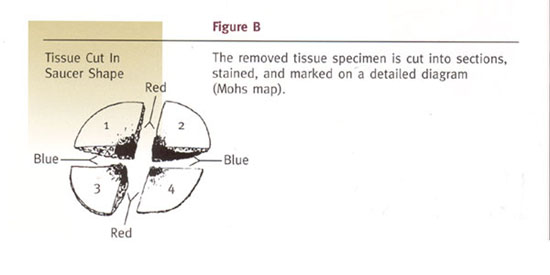
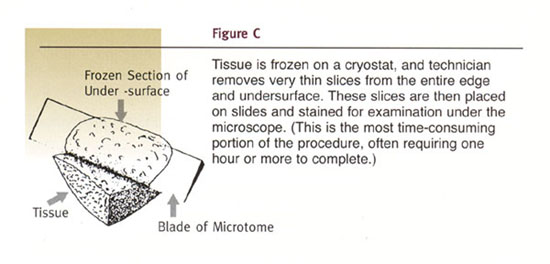
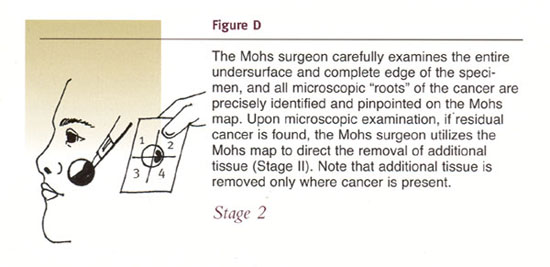
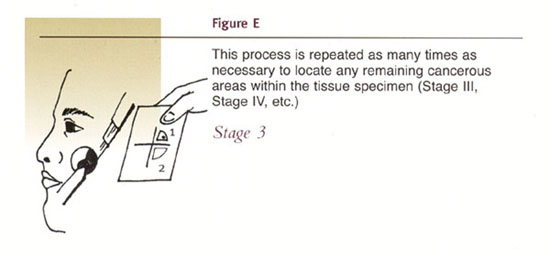
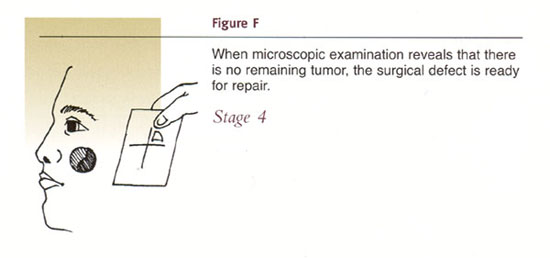
The Mohs Surgical Procedure
Dr. Sekula Gibbs typically performs Mohs surgery as an outpatient procedure
in the surgical suites of her Webster office (in the Clear Lake area). Although the patient is awake during
the entire procedure, discomfort is usually minimal and no greater
than it would be for more routine skin cancer surgeries. The
Mohs surgical procedure is illustrated in the following diagrams.
Insurance Coverage for Mohs Surgery
Most insurance policies cover the costs of Mohs surgery and
the reconstruction of the resultant surgical area. Please contact
your insurance carrier directly for the most current payment
information relative to this surgery. The insurance billing
department in our office will be able
to assist you.
Patient Preparation for Surgery
It is important that you obtain a good night’s rest and
eat normally on the day of the surgery. If you are taking prescription
medications, continue to take these unless otherwise directed
by Dr. Sekula GIbbs. However, you should avoid taking aspirin-containing
medications for ten days prior to your surgery. You also should
avoid aspirin substitutes (such as Advil, Motrin, Naprosyn,
etc.) within seventy-two hours of surgery. If you are taking coumadin or other blood thinners, please discuss stopping it with Dr. Sekula Gibbs and your prescribing physician. Tylenol, however,
may be taken at any time prior to surgery. For your comfort,
it is recommended that you wear casual, layered clothing on
the day of your surgery. You may also wish to bring a light
snack and a book or magazine to help occupy your waiting time.
Also, it is highly recommended that you arrange for someone
to drive you home following surgery.
Duration of Procedure
Most Mohs cases can be completed in three or fewer stages,
requiring less than four hours. However, it is not possible
to predict how extensive a cancer will be, as the extent of
a skin cancer’s “roots” cannot be estimated
in advance. Therefore, it is advisable to reserve the entire
day for this surgical procedure, in case the removal of additional
layers is required.
Minor Post-Surgical Discomfort Expected
Most patients do not complain of significant pain. If there
is some discomfort, normally only Tylenol is required for relief.
However, stronger pain medications are available and will be
prescribed when needed. You may experience some bruising and
swelling around the wound, especially if surgery is performed
near the eye area.
Options for Post-Surgical Reconstruction
After the skin cancer has been removed, Dr. Sekula Gibbs will
discuss the following options with you:
- Allowing the wound to heal naturally, without the necessity
of additional surgery (which may produce the best cosmetic
result).
- Simple or complex wound repair performed by the Mohs
surgeon either on the day of surgery or a week after the surgery.
- Referral to the original referring physician for wound
repair.
- Referral to another surgeon for wound repair.
If your wound requires daily care at home, you will be given
detailed instructions following your surgery. For small post-surgical
sites, direct closure by suturing the sides of the wound together
may be possible. However, in certain areas of the body, there
is very little tissue that can be stretched for coverage of
a wound, and either a skin graft or skin flap must be used.
In closing wounds with a skin flap, the skin adjacent to the
surgical defect is partially cut free, and then rotated or moved
forward to cover the surgical area. Stitches are then placed
to hold the flap in its new position. This provides immediate
coverage for the wound. Other areas may require a skin graft
to provide coverage. Skin from the side of the neck, behind
the ear, or over the collarbone may be cut free, placed over
the wound, and then sewn into place. The original site of the
graft is then closed with stitches or allowed to heal on its
own.
Wound Healing, Scarring, and Scar Revision
As with all forms
of surgery, a scar will remain after the skin cancer is removed
and the surgical area has completely healed. Mohs micrographic
surgery, however, will leave one of the smallest possible surgical
defects and resultant scars. Often, wounds allowed to heal on
their own result in scars that are barely noticeable. Even following
extensive surgery, results are frequently quite acceptable.
In addition, scars do have the ability, through the body’s
own natural healing properties, to remodel and improve in appearance
for a six to twelve month period. There are also many other
techniques available to the patient for enhancement of the surgical
area following skin cancer surgery. Depressed or indented scars
may be elevated, using an implant such as collagen or hyaluronic acid. Likewise,
a raised or roughened scar may be smoothed, using laser resurfacing
or chemical peeling techniques. Skin flaps and grafts also may
require a subsequent “touch up” procedure, to further
improve their appearance.
Potential Complications Associated With Mohs Surgery
Patients should understand that there is not an absolute guarantee
that any given procedure will be totally free of complications
or adverse reactions. Mohs surgery is no exception. During surgery,
tiny nerve endings are cut, which may produce a temporary or
permanent numbness in and around the surgical area. If a large
tumor is removed or extensive surgery is required, occasionally
a nerve to muscles may be cut, resulting in temporary or permanent
weakness in a portion of the face. This is, however, an unusual
complication. The surgical area may remain tender for several
weeks or months after surgery, especially if large amounts of
tissue were removed. Rarely, some patients experience intermittent
itching or shooting pain in the surgical area. In addition,
the skin grafts and flaps used to cover surgical areas may not
fully survive, requiring additional repair.
|
|